Introduction
Wet AMD can be treated, and there are a growing number of effective treatment options available. In the past, the only way to seal leaking blood vessels in wet AMD was using a laser in a procedure called Laser Photocoagulation. In the 1990s, a treatment called Photodynamic Therapy (PDT) was developed using Visudyne™ (a drug injected into the bloodstream that is activated by the laser when it passes into the affected area of the eye).
Beginning in 2004, an even more effective type of treatment, called “Targeted Therapy” was developed. These latest treatments take aim at the specific protein, VEGF, which causes abnormal new blood vessels to form through the process of angiogenesis in wet AMD. Treatments called anti-VEGF therapies have now revolutionized the treatment of wet AMD, saving vision and maintaining quality of life for millions of people around the world.

Clinical Outcomes
Treatments aimed at angiogenesis (new blood vessel growth) in the eye are called “antiangiogenic therapies”. They are also called “anti-VEGF therapies” because the treatments aim at a protein called VEGF found to be a primary cause of blood vessel growth in the eye. Anti-VEGF therapies can slow the progression of AMD and in some cases improve vision. The treatments are only beneficial, however, when they are used before scar tissue and irreversible vision loss develops.
Antiangiogenic Treatments
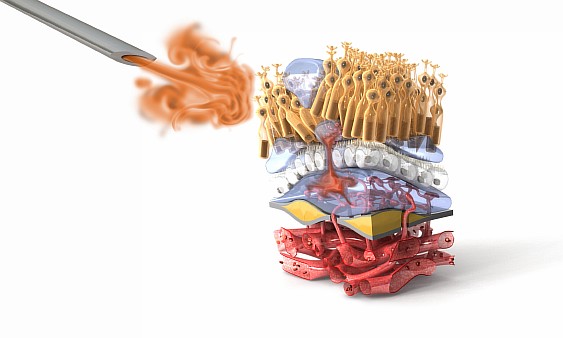
VEGF (Vascular Endothelial Growth Factor) is a protein that triggers new blood vessel formation in the eye by activating the cells lining normal blood vessels. These cells are called endothelial cells.
In wet AMD, VEGF is produced at higher than normal amounts in the retina. Excess VEGF prompts the growth of new blood vessels beneath the macula. These vessels are abnormal and leak fluid or even blood into the delicate tissues within the eye, damaging the macula and causing the loss of central vision.
Anti-VEGF therapies are drugs designed to reduce levels of the VEGF protein. Such treatments stop new blood vessels from growing, decrease the leaking fluid, and prevent bleeding, thereby saving vision.
There are five different VEGF inhibitors that have been proven to be effective for wet AMD:
- Macugen (Pegaptanib) – First VEGF inhibitor to be approved to treat wet AMD
- Lucentis (Ranibizumab) – Widely prescribed treatment for wet AMD
- Eylea (Aflibercept) – Approved in the United States to treat wet AMD and targets two angiogenesis factors
- Avastin (Bevacizumab) – Cancer drug with anti-VEGF activity that has been used off-label by Retinal Specialists to treat wet AMD
- Beovu (brolucizumab) – Recently approved in the U.S. and Europe to treat wet AMD with potentially less frequent dosing
All anti-VEGF therapies for wet AMD are injected into the eye by a Retinal Specialist. Retinal Specialists are trained to perform this simple procedure so as to minimize pain and risk. The frequency of treatment is determined by the Retinal Specialist based on your condition.
Anti-VEGF therapies are all relatively safe treatments when given by trained Retinal Specialists. All drugs, however, have risks that need to be balanced with their benefits. For anti-VEGF therapies, those risks include:
- Eye infection
- Increased eye pressure
- Retinal detachment
Wet AMD is generally considered a chronic disease that requires lifelong monitoring and treatment. With the current anti-VEGF therapies, regular continuous treatments seem to be required to maintain control over angiogenesis and to preserve vision. If treatments are not followed according to the Retinal Specialist’s orders, vision may deteriorate and irreversible blindness may result. The length and frequency of treatment should be discussed with your Retinal Specialist.
References
Macugen
Macugen is an aptamer (a short chain of nucleotides) that specifically targets VEGF, developed for the treatment of wet AMD. It is injected directly into the eye. Macugen helps to slow vision loss but generally does not improve vision. Macugen is administered in 0.3 mg doses once every six weeks by injection directly into the eye.
Data from clinical trials involving 1,200 patients with wet AMD have shown that more than half of individuals treated with Macugen lost fewer than three lines of visual acuity on the eye chart over the first year of the study. Macugen stabilizes vision in approximately 65% of people.
Commonly reported adverse events with Macugen include: inflammation, blurred vision, conjunctival hemorrhage, eye irritation, eye pain, floaters, and increased eye pressure. Serious complications of injections in the eye include endophthalmitis (infection) and retinal detachment.
References
Lucentis
Lucentis is a type of anti-VEGF drug called a monoclonal antibody fragment that was developed to treat retinal diseases. It is injected directly into the eye, and can stabilize or even improve vision loss. According to the Lucentis package label, best results occur when 0.5 mg of Lucentis is given every month. Some Retinal Specialists give Lucentis less frequently than every month.
Data from clinical trials involving more than 1,300 people have shown that after two years of treatment, monthly injections of 0.5 mg of Lucentis stabilizes vision for an estimated 90% of patients (their vision did not get significantly worse). Vision improved significantly for approximately 30% of treated patients.
Commonly reported side effects of Lucentis injections include conjunctival hemorrhage, eye pain, floaters, increased eye pressure, and inflammation of the eye. Serious complications of injections in the eye include endophthalmitis (infection) and retinal detachment.
References
Eylea
Eylea is a type of anti-VEGF drug known as a fusion protein and is directly injected into the eye to treat wet AMD. Eylea targets VEGF, as well as another protein called Placental Growth Factor (PlGF), which has also been found in excess amounts in the retina of people with wet AMD. After 3 monthly injections, injections of Eylea every other month show comparable effectiveness with monthly injections of Lucentis.
Clinical trials of about 2,400 people with wet AMD compared monthly 0.5 mg injections of Lucentis with injections of 2 mg Eylea given monthly for three months, and then given every other month. After one year of treatment, bimonthly Eylea was shown to improve or maintain vision in AMD patients at a level comparable to monthly Lucentis. The safety of both drugs was also comparable. Overall, patients who were given Eylea needed fewer injections to achieve the safe effectiveness as monthly injections of Lucentis.
Commonly reported side effects of Eylea include conjunctival hemorrhage, retinal hemorrhage, and reduced visual acuity. Serious complications of injections in the eye include endophthalmitis (infection) and retinal detachment.
References
Beovu
Beovu is a small-sized, single strand antibody fragment with enhanced tissue penetration and active drug binding, that delivers a high concentration of the anti-VEGF drug to the target area in the eyes of patients with wet AMD. Beovu allows for 3-month dosing intervals after a 3-month loading phase, which may offer benefit to patients on other anti-VEGF drugs that require four week dosing periods, and for which frequency of monthly injections creates a burden. In two Phase III clinical trials, Beovu was effective in half of the patients at a dosing interval of 12 weeks in between treatments; the other half required treatments at 8-week intervals.
On average, patients gained seven letters on the eye chart, and 30 percent of patients gained at least 15 letters. In the trials, Beovu given every 2-3 months was non-inferior to Eylea given every two months. In addition, those patients receiving Beovu had reduced central retina thickness, and less retinal fluid detectable by OCT imaging.
References
Off-label Therapy
Avastin
Avastin is a type of anti-VEGF drug called a monoclonal antibody developed for the treatment of cancer (which also depends upon angiogenesis for disease progression). Avastin is the molecule from which Lucentis is derived. Some Retinal Specialists treat wet AMD patients with Avastin which has been diluted and repackaged to be injected directly into the eye. Since Avastin injections seem to be similar to Lucentis in how well they treat wet AMD, some Retinal Specialists use Avastin because it is significantly less expensive than Lucentis. Avastin 1.25 mg injections can be given monthly or less often, on a schedule determined by the Retinal Specialist.
Since Avastin has not been approved by the FDA to be used in the eye, the U.S. National Institutes of Health conducted a clinical trial called the Comparison of AMD Treatment Trial (CATT) study for about 1,200 people with wet AMD. The CATT study compared the safety and effectiveness of Avastin 1.25 mg injections with Lucentis 0.5 mg injections. To date, only one year of results are available. The study found that Avastin injections on the same dosing schedule as Lucentis were similar in effectiveness. The common side effects of the two drugs were similar. People treated with Avastin had more serious side effects in this trial, however, this connection has not been definitively proven.
Serious complications of injections in the eye include endophthalmitis (infection) and retinal detachment.
References
Implantable Telescope
Implantable Telescope
The Implantable Miniature Telescope (IMT) was FDA-approved in July 2010 for end-stage AMD. This device is manufactured by VisionCare Ophthalmic Technologies Inc. of Saratoga, California, and its approval followed a 219-patient, multi-center clinical study in which 90 percent of patients achieved at least a 2-line gain in either their distance or best-corrected visual acuity, and 75 percent their level of vision from severe or profound impairment to moderate impairment.
Patients 75 years or older with stable to severe profound vision impairment due to blind spots (bilateral central scotoma) are now eligible for surgical implantation of this device, which projects images at greater than two times magnification onto the retina to improve central vision. Options are available for 2.2 and 2.7x magnification. Pre-training with an external telescope with a low vision specialist is required prior to procedure to ensure the device can have a benefit, as well as to determine eligibility (inadequate peripheral vision). Post-op visual training is required, as well.
One risk of this device includes the loss of corneal endothelial cells, which are essential for maintaining corneal clarity. The degree of this loss can be chronic (up to 5 percent per year). Major losses may have negative downstream effects, including corneal edema (swelling), decompensation (further loss of function), and ultimately a need for corneal transplant. 10 eyes in the above named study had corneal edema (unresolved), half of which resulted in corneal transplant. Calculated 5-year risks for adverse outcomes were calculated as follows: corneal edema (9.2 percent), corneal decompensation (6.8 percent) and corneal transplant (4.1).
Two post-approval studies are being carried out to further delineate risk, including a two-year follow up of the study’s initial two year cohort as well as a novel study of 770 newly enrolled subjects (focusing on endothelial cell density and related sequelae). Measures were also taken to ensure patients are informed of risks, including detailed labeling (manufacturer and FDA-generated) and an Acceptance of Risk and Informed Decision Agreement.
Visudyne
Visudyne (photodynamic therapy)
Photodynamic therapy with Visudyne injection was FDA-approved in 2000 for the treatment of age-related macular degeneration (predominantly classic subfoveal choroidal neovascularization). Alternate indications include pathologic myopia or presumed ocular histoplasmosis. This drug is activated by light, and functions to block the mature vessels that may be expressing less or no VEG-F, contributing to persistent AMD activity in spite of anti VEG-F treatments.
The most common adverse events reported with Visudyne include injection site reactions, blurred vision, decreased visual acuity and visual field defects (10-30%). Contraindications include porphyria or known hypersensitivity to any component of the drug formulation.
Macular Translocation Therapy
Macular Translocation Therapy
Macular translocation therapy is a surgical intervention for wet AMD only, and involves detaching and rotating the retina, such that placement will allow the macula to sit on a new, healthy base. It is not used for dry AMD due to degeneration occurring in the retina’s new position. Eligibility entails central vision loss in both eyes, with one having developed the condition in the preceding 6 months. It has been shown to be effective for some when performed promptly.3
Complications include cataract formation, infection, intraocular bleeding, retinal detachment and/or tears and total vision loss. Since retinal rotation causes tilted or double vision, a second correction surgery for eye muscles is required 2 months after the initial procedure. Both are performed on an outpatient basis.
References